Anemia Iron-Deficiency Anemia
What is iron-deficiency anemia?
Iron-deficiency anemia is a type of anemia that develops if you do not have enough iron in your body. It is the most common type of anemia.
What are the symptoms of iron-deficiency anemia?
People with mild or moderate iron-deficiency anemia may not have any symptoms. More serious iron-deficiency anemia may cause common symptoms of anemia, such as tiredness, shortness of breath, or chest pain. Other symptoms include:
- Fatigue
- Dizziness or lightheadedness
- Cold hands and feet
- Pale skin
What causes iron-deficiency anemia?
Your body needs iron to make healthy red blood cells. Conditions that increase your risk of iron-deficiency anemia include the following:
Blood loss
When you lose blood, you lose iron. Blood loss can happen in many ways:
- Bleeding in your (GI tract) from an inflammatory bowel disease, ulcer, colon cancer, or a or other GI disorders such as celiac disease.
- Traumatic injuries or surgery
- Heavy menstrual periods or bleeding during childbirth
- Regular use of medicines such as aspirin or nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen and naproxen that can lead to GI tract bleeding
- Urinary tract bleeding
Problems absorbing iron
Certain conditions or medicines can decrease your body’s ability to absorb iron and lead to iron-deficiency anemia. These conditions include:
- Certain rare conditions that block your intestines from absorbing iron or make it harder to stop bleeding
- Endurance sports, which can make athletes lose iron through their GI tracts and through the breakdown of red blood cells
- Intestinal and digestive conditions, such as celiac disease, ulcerative colitis, Crohn’s disease, and Helicobacter pylori infection
- Surgery on your stomach and intestines, including weight loss surgery
Other medical conditions
Other conditions that may cause iron-deficiency anemia include:
- Kidney disease: People who have kidney disease do not make enough of a substance called erythropoietin. Your body needs erythropoietin to make red blood cells. Your doctor may prescribe erythropoietin if you have kidney disease.
- Long-lasting conditions that lead to inflammation: These include congestive heart failure or obesity. They can make it hard for your body to regulate and use your body’s iron.
Sometimes young children can develop iron-deficiency anemia if they do not get enough iron in their diet. This usually occurs between the ages of 9 months and 1 year, as a child transitions to eating whole foods.
How do you prevent iron-deficiency anemia?
Iron-deficiency anemia may be preventable if you are able to treat the causes of blood loss or problems with iron absorption that can lead to the condition.
It is also always a good idea to help the body keep iron levels where they need to be by maintaining a healthy diet that includes good sources of iron and vitamin C.
- Good sources of iron include beans, dried fruits, eggs, lean red meat, salmon, iron-fortified breads and cereals, peas, tofu, and dark green leafy vegetables.
- Vitamin C-rich foods such as oranges, strawberries, and tomatoes help your body absorb iron.
- Ensure that toddlers eat enough solid foods that are rich in iron.
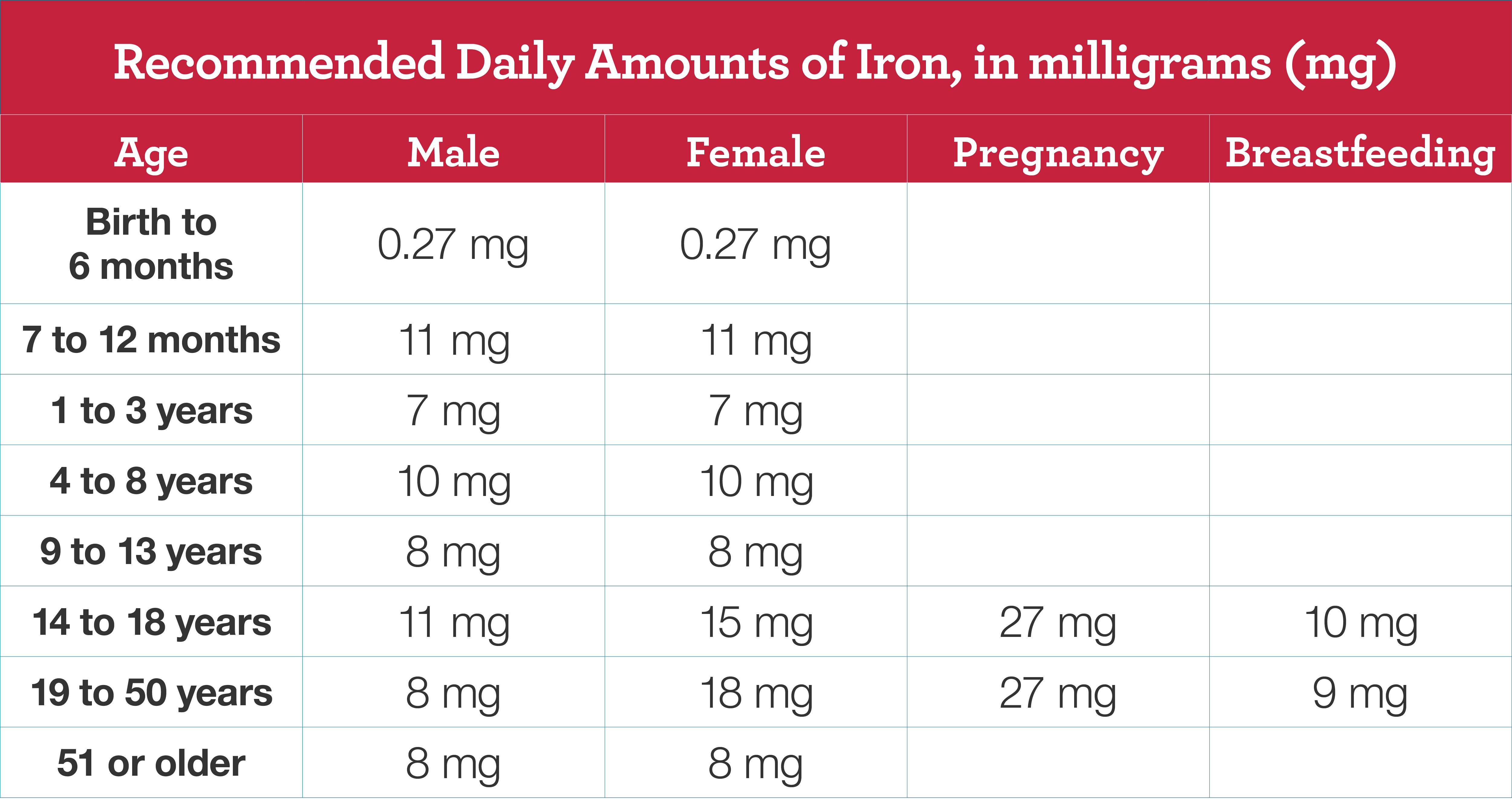
How much iron do I need each day?
The recommended daily amounts of iron depend on your age, your sex, and whether you are pregnant or breastfeeding.
Generally, a diet that includes beans, dried fruits, eggs, lean red meat, salmon, iron-fortified breads and cereals, peas, tofu, and dark green leafy vegetables will provide the iron level that your body needs.
Recommended daily iron intake for children and adults
How is iron-deficiency anemia diagnosed?
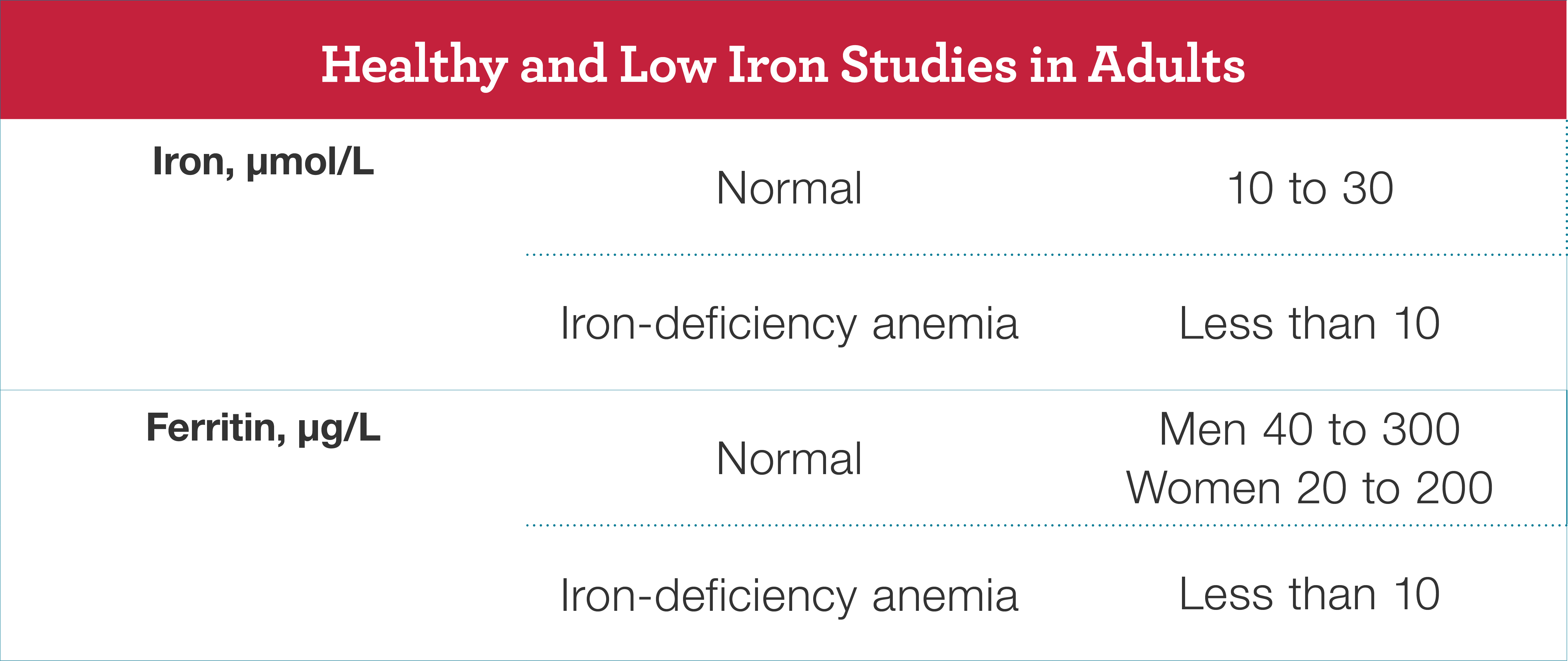
To help diagnose iron-deficiency anemia, your doctor will order a blood test to check your complete blood count (CBC), hemoglobin levels, blood iron levels, and ferritin levels. Your doctor may tell you that the iron level in your blood is low. Your doctor may also tell you that you have anemia with the iron deficiency.
How is iron-deficiency anemia treated?
Several treatments can be used to treat anemia.
- Iron supplements, also called iron pills or oral iron, help increase the iron in your body. This is the most common treatment for iron-deficiency anemia. It often takes three to six months to restore your iron levels. Your doctor may ask you to take iron supplements during pregnancy. Talk to your doctor if you have side effects such as a bad metallic taste, vomiting, diarrhea, constipation, or upset stomach. Your doctor may suggest taking your supplements with food, lowering the dose, or trying a different type of iron supplement.
- Intravenous or IV iron is sometimes used to put iron into your body through one of your veins. This helps increase iron levels in your blood. It often takes only one or a few sessions to restore your iron levels. People who have serious iron-deficiency anemia or who have long-term conditions are more likely to receive IV iron. Side effects include vomiting or headaches right after the treatment, but these usually go away within a day or two.
- Medicines such as help your bone marrow make more red blood cells, if this is causing your iron deficiency. These medicines are usually used with iron therapy in people who have both iron-deficiency anemia and another chronic (long-term) condition such as kidney disease.
- Blood transfusions quickly increase the amount of red blood cells and iron in your blood. They may be used to treat serious iron-deficiency anemia.
- Surgery may be needed to stop internal bleeding.
In addition to the steps above, your doctor may ask you to adopt heart-healthy eating habits and to choose iron-rich foods such as beans, dried fruits, eggs, lean red meat, salmon, iron-fortified breads and cereals, peas, tofu, and dark green leafy vegetables. Foods that are rich in vitamin C can help your body absorb iron. Some foods like black tea can reduce iron absorption.
What happens if iron-deficiency anemia is not treated?
Undiagnosed or untreated iron-deficiency anemia may cause serious complications such as fatigue, headaches, restless legs syndrome, heart problems, pregnancy complications, and developmental delays in children.
Iron-deficiency anemia can also make other chronic conditions worse or cause their treatments to work poorly.

